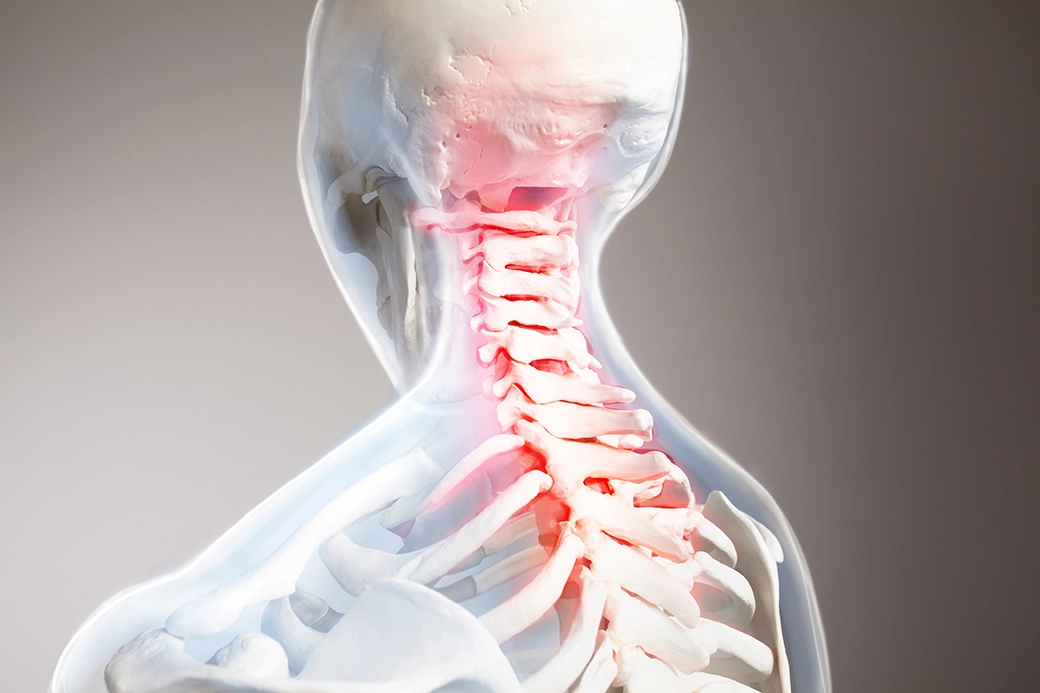
If you suffer from cervical radiculopathy, the first thing you want to do is make sure it doesn’t get worse – because it can be painful!
The thing that is most likely to make cervical radiculopathy worse is usually a worsening of the underlying condition that caused it in the first place. Most of the time, this is the worsening of foraminal stenosis or a cervical herniated disc. However, there are a few other possibilities.
Let’s look into this more deeply.
Cervical radiculopathy is most often caused by either cervical foraminal stenosis or a cervical herniated disc. As a result, if the cervical radiculopathy of an individual is caused by one of these conditions, the worsening of that underlying condition will likely, in turn, worsen the cervical radiculopathy as well.
A foramen is a small opening in the spine that lets a nerve exit the spinal canal. Cervical foraminal stenosis is a condition where this opening becomes progressing narrower and narrower. At some point, it will begin to impinge upon the nerve that exits through it. When this happens, radiculopathy (pain radiating along the nerve to parts of the body different from the point of origin) may result. Obviously, as the foramen continues to shrink, the impingement will increase, as will the severity of radiculopathy.
A herniated disc, on the other hand, is a disc whose outer wall has been ruptured allowing the gel-like interior to squeeze out and contact a nerve. This contact can irritate the respective nerve sending pain signals along its length (radiculopathy). If more gel extrudes, the irritation will worsen. In the case of cervical radiculopathy, the disc in question is located in the neck. But the pain may be felt in the shoulder, arm, wrist, or other locations.
Other less common causes of cervical radiculopathy include:
- Tumors
- Injury/Fracture
- And Infection
All three of these can lead to a worsening of cervical radiculopathy if the underlying cause itself worsens. For example, if tumors are causing a narrowing in the foramen of the cervical spine, an increase in tumors may likely increase that narrowing leading to a worsening case of radiculopathy.
Other potential factors that can lead to a worsening of cervical radiculopathy include:
- Age: Naturally, as you get older your spine and other skeletal structures age as well. In cases, where the cause of cervical radiculopathy can be traced back to the degeneration of the spine from age, it will likely worsen as time progresses.
- Strenuous Exertion Involving the Neck: This can include sports like wrestling and some types of weightlifting. Stressing the neck can lead to injury or issues that ultimately result in cervical radiculopathy and can make it worse, if already present.
Other less obvious factors that can worsen cervical radiculopathy are usually related to poor lifestyle choices. These include:
- Smoking
- Obesity
- A sedentary lifestyle
- Sleeping on your stomach
In the end, though, the most pernicious culprit behind the worsening of cervical radiculopathy is usually time. As noted above, age can have a significant contribution to the development of skeletal issues. The spine tends to degenerate over time. And this can lead to the worsening of many conditions, not just cervical radiculopathy.

Treating Cervical Radiculopathy
As far as treating cervical radiculopathy, the science suggests that it is best to start with conservative measures before trying heavy-duty measures like surgery or potent painkillers.
A study in the Journal of Neurosurgery found that “in patients in whom symptoms of cervical radiculopathy were present for approximately 6 weeks that 75% will respond to further conservative treatment (halter traction and cervical collar) over the next 6 weeks.” (1)
Another study from Sage Journals found that “Most patients will significantly improve from non-surgical active and passive therapies.” (2)
For a more concrete example, a case study in the Journal of Manipulative and Physiological Therapeutics on Science Direct involving a 33-year old man with neck pain and radiculopathy found that “Cox flexion distraction decompression manipulation and physiotherapy modalities showed good subjective and objective clinical outcomes for this patient.”(Cox flexion distraction is a type of chiropractic therapy). (3)
Another case study in the Journal of Chiropractic Medicine on Science Direct described a 64-year old man who was successfully treated for multiple ailments including cervical radiculopathy originating from a herniated disc. The patient was “pain-free and fully function 8 months following the conclusion of care.” (4)
Cervical Radiculopathy Flare Ups
Cervical radiculopathy comes in varying levels of severity. For some people, symptoms are not present on a regular basis. Instead, the individual in question experiences periodic flare-ups where they feel pain or tingling sensations in their hand or arm that leaves after a short period of time. The problem is that it will come back.
One way to deal with such an issue is to use medications, such as NSAIDS (non-steroidal anti-inflammatory drugs), to cope with individual incidents. However, if the flare-ups are getting worse, and you find yourself taking more and/or more potent medications as time goes on, you might want to seek out some other medical assistance.
Over the long term, it would be a good idea to find a chiropractor or physical therapist to help you implement a conservative treatment plan or make appropriate lifestyle changes.
How To Calm Cervical Radiculopathy?
Of course, if you have a flare up, you want immediate relief. Although such is not always possible, there are a number of exercises to try, like shoulder-blade squeezes for example, that might help bring some immediate relief by reducing tension in the neck and surrounding muscles.
Another option is the medications we mentioned above (NSAIDS and whatnot).
Over the long-term though, you’ll likely need to implement lifestyle changes (usually best done under the care of a chiropractor or other medical professional). Such changes can involve sleeping habits. For example, sleeping on your back instead of your stomach should go a long way in reducing neck issues.
There are also special cervical pillows that can be used to make your sleep more comfortable. They are designed with neck issues in mind and they can be purchased from drug stores, chiropractic offices, and physical therapist offices. They, too, should help.
When To See A Chiropractor For Cervical Radiculopathy?
The best answer to this question is that you should see a chiropractor for cervical radiculopathy as soon as you find out you have it, or as soon as you start suffering symptoms that indicate you have some kind of musculoskeletal issue going on.
A study in Muscle & Nerve on the Wiley Online Library found that the symptoms of cervical radiculopathy can mimic and be mimicked by a number of different diseases, including: neck tension, cervicogenic headache, rotator cuff tears/impingement, and many more. So, it’s important to get a diagnosis by a professional. (5)
A chiropractor can perform or order a cervical radiculopathy test to give you an accurate diagnosis. Once you have that, then your chiropractor can develop a treatment program to deal with the issue.
Chiropractors are well-suited to deal with cervical radiculopathy because they are experts on both the nervous system and the musculoskeletal system. One of the many tools at a chiropractor’s disposal is the chiropractic adjustment. This is where the chiropractor, using the strategic application of pressure with his hands, can shift and adjust the position of bones and vertebrae in the body.
There are a number of benefits from getting a chiropractic adjustment – not just pain relief, reduction in tension, and improvement of posture. Over the long term it can improve the immune system and help deal with many medical diseases.
Conclusion
Ultimately, the best way to prevent worsening of cervical radiculopathy is to be proactive about it. Seek out a qualified medical professional, like a chiropractor or physical therapist, and let them develop a plan of care for you and your condition.
- https://thejns.org/focus/view/journals/neurosurg-focus/12/2/foc.2002.12.2.4.xml
- https://journals.sagepub.com/doi/abs/10.1007/s11420-011-9218-z?journalCode=hssa
- https://www.sciencedirect.com/science/article/abs/pii/S0161475408001085
- https://www.sciencedirect.com/science/article/abs/pii/S1556370711001593
- https://onlinelibrary.wiley.com/doi/abs/10.1002/mus.27553